TeleLink Mental Health
TeleLink is a program that provides a virtual mental health consultation service for children and youth in partnership with their caregivers. We connect children/youth, caregivers, and care teams to mental health specialists using virtual technology so they don’t have to leave their community.
Patient care is individualized to meet the needs of the child or youth and can include teachers, case managers, doctors, nurse practitioners and others as determined by the referral team. We also provide agencies with program consultations or education sessions on a variety of topics aimed at building capacity and increasing knowledge.
Areas of expertise
The TeleLink team, within the Division of Child Psychiatry at the University of Toronto, is comprised of child psychiatrists, social workers, nurse practitioners, psychologists and administrative staff. They provide a range of expertise on topics such as:
- Attention Deficit Hyperactivity Disorder (ADHD)
- Disruptive behaviour disorders
- Mood and anxiety disorders
- Learning difficulties
- Attachment disorders
- Autism Spectrum Disorders (ASD)
- Psychosis/thought disorders
- Transgender
- Eating disorders
- Other
Main services offered
- Direct clinical consultations for children/youth under 18 years old
- Program consultations for agencies aimed at capacity building
- Education sessions/series for agencies on a variety of topics
- Services offered in both English and French
- Partnerships with Indigenous liaisons to provide culturally sensitive service
- Interpretation services (free of charge) in any language
- No fee for service; must be a resident of Ontario
-
We are a consultative and capacity building service for community primary care providers and do not provide ongoing direct client/patient care.
More TeleLink services
TeleLink also supports remote areas outside of Ontario, including Nunavut and the Northwest Territories. Team members are licensed to offer care in these other areas of Canada, to ensure that mental health services are available to these remote communities. The partnerships provide the same services to these territories through a common referral pathway.
Telepsychology (virtual psychological services) are also offered by the TeleLink program to rural children’s mental health centres. The Telepsychology program works closely with psychometrists from a variety of remote regions to ensure reliable test administration, quality of service, clinical consultation, supervision and capacity building to under-served populations.
What we do
Our main referral pathway via the Tele-mental Health Service (TMHS) is funded by the Ministry of Health and offered free of charge to Ontario residents under the age of 18.
Sickkids collaborates with the Children’s Hospital of Eastern Ontario (CHEO) and Vanier Children's Mental Wellness to provide consultations to rural, remote or underserviced areas with expert mental health supports.
Who can refer?
Referrals via the Tele-mental Health Service (TMHS) pathway can come from:
- Child and youth mental health agencies
- School boards
- Hospital outpatient programs
- Family health teams
- Aboriginal health access centres
- Friendship centres
- Youth justice settings
- Other community-based agencies that provide child and youth mental health services in Ontario
How can you refer?
The TMHS has partnerships with coordinating agencies across Ontario that help to support youth and their families access resources within their own communities. These coordinating agencies also help families connect with specialist services like ours when needed. Referrals should be directed to the coordinating agency dedicated to your service area.
Three service agencies are dedicated to the general population (see map below):
- HANDS Child and Youth Mental Health - The Family Help Network
- Woodview Mental Health and Autism Services
- Algoma Family Services
Three overlapping agencies are dedicated to First Nation, Metis, Inuit and urban Aboriginal populations (see map below):
- Southwest Ontario Aboriginal Health Access Service
- Dilico Anishinabek Family Care
- Weechi-it-te-win Family Services
For agencies referring within Toronto/GTA (Urban), please direct referrals to:
Service maps
Please direct general population referrals to the Coordinating Agency servicing your community.
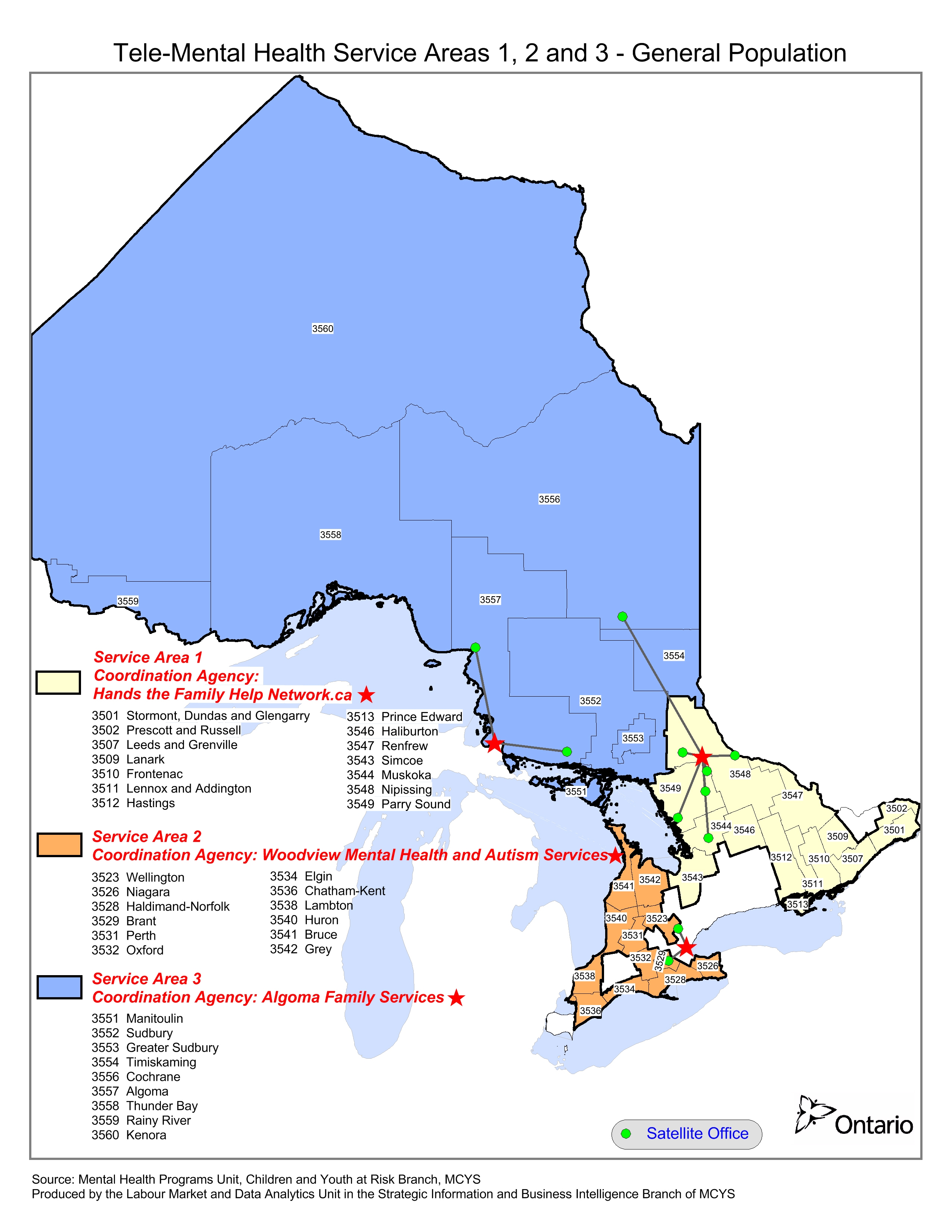
Map of service area 1: Northeastern Ontario; service area 2: Southwestern Ontario; and service area 3: Northwestern Ontario.
Please direct First Nations, Inuit, Metis and urban Aboriginal population referrals to the Coordinating Agency servicing your community.
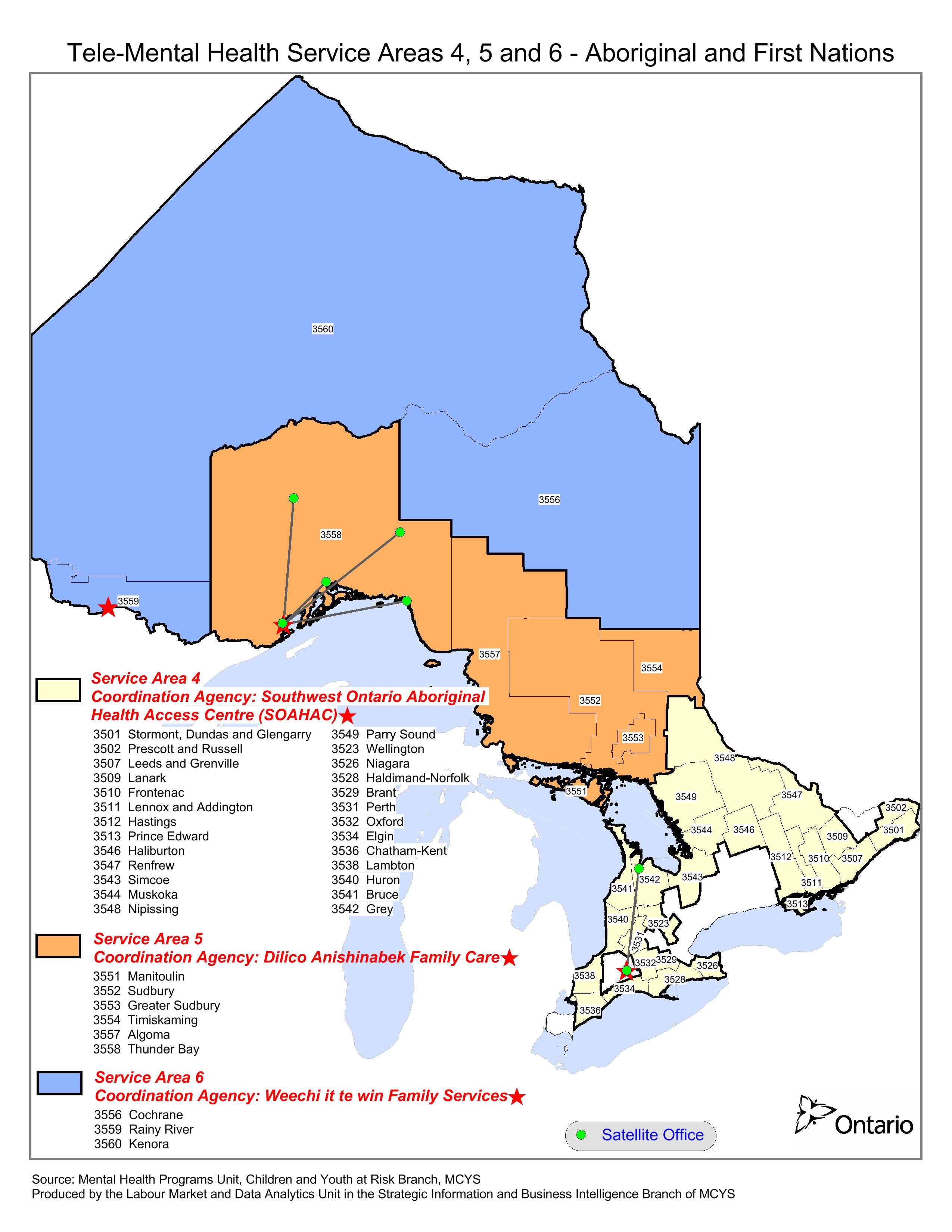
Map of First Nations service area 4: Southwestern Ontario; service area 5: West Ontario; and service area 6: Northwestern Ontario.
Clinical consultation is when one of our mental health professionals provide a mental health assessment with children or youth, their caregivers and their mental health team. We highly recommend inclusion of case workers/managers, or the primary care team be present during the consult to ensure that recommendations can be implemented and followed. Referrals are triaged by presenting issue and urgency and matched to compatible consultants. For non-urgent referrals, the average time from referral to initial consultation is approximately six to eight weeks.
Program Consultation is a capacity building platform for community agencies to allow them access to expert mental health providers to consult on clinically relevant cases and topics. A consultant meets monthly with a designated group of mental health providers to discuss clinical, program-wide and community issues. Topics discussed may include individual youth and their emotions and behaviours, diagnosis, formulation and management. Consultants offer education, support, and guidance when working with very difficult or complex situations. Every program consultation is tailored to the specific need of the program and local community.
To submit a program consult request, please complete a request form.
Education sessions can cover a wide range of clinical topics and can be delivered as a one-time session or presented as an education series. Sessions are geared to the needs of the requesting agency and can be either an introductory or advanced level to meet the needs of the diversity of practitioners at community agencies. Utilizing virtual platforms allows us to provide education to a wide audience without the added travel costs; any of our mental health providers can deliver education and training.
To request an education session, please complete a request form.
Consent for Release of Information
Consent is required for a report to be sent to any referral sources. The form should be signed by the patient (if deemed capable) for the release of their health information.
TMHS Referral Forms (English)
- TeleMental Health Referral Form (PDF)
- TeleMental Health Follow Up/Second Opinion Request Form (PDF)
- TeleMental Health Consent to Disclosure Form (PDF)
TMHS Referral Forms (French)
Please note that written recommendations will be provided in English.
- Formulaire de référence (PDF)
- Formulaire de suivi et demande d’un deuxième avis (PDF)
- Formulaire de consentement à la divulgation de renseignements personnels sur la santé (PDF)
Alternative referral pathway
A direct referral from a primary care provider (Physician or Nurse Practitioner) to the TeleLink program will be accepted by our service. This pathway requires a valid Ontario health card number be provided for service.
Referrals are submitted via eCHN.
Who we are
The mental health team at TeleLink strives to provide excellence in our service. The administrative team works closely with community partners to ensure timely action for all referrals. We strive to have an appointment offered with 48 hours and work to meet the needs of the patients, caregivers and agencies that we partner with to provide seamless virtual mental health care.
TeleLink is committed to matching community needs with best evidence and excellence in care through partnership and evaluation to build capacity in our community agencies and foster meaningful collaborations with stakeholders. We strive to acknowledge cultural diversity and are inclusive of all who need our services.
A teaching hospital
Operated under the auspices of The Hospital for Sick Children, TeleLink is fully affiliated with the University of Toronto, as a program with the Division of Child and Youth Mental Health in the Department of Psychiatry.
Key staff
Expand the section below for a list of consultants, including short biographies.
Read our Tele-Mental Health Consultant Bios (PDF), or see below for a full list at each Hub.
SickKids Consultants:
- Dr. Farid Ahmad
- Dr. Tatyana Barankin
- Dr. Peter Braunberger, Liaison to Indigenous Communities
- Dr. Pier Bryden
- Dr. Clive Chamberlain
- Dr. Claire DeSouza
- Dr. Susan Dundas
- Dr. Jennifer Felsher, C.Psych
- Dr. Mark Hanson
- Dr. Abel Ickowicz
- Dr. Nicola Keyhan
- Dr. Upasana Krishnadev
- Dr. Chetana Kulkarni, Education Lead
- Janine Lawford, MSW RSW
- Dr. Greg Lodenquai
- Dr. Donna MacLachlan
- Dr. Arfeen Malick
- Dr. Cecilia Marino
- Dr. Irfan Mian
- Dr. Suneeta Monga
- Dr. Tony Pignatiello, Medical Director
- Dr. Priya Raju
- Dr. Moni Ravi
- Dr. Dafni Sadler
- Dr. Janet Song
- Charlie Wharton, NP
- Dr. Jean Wittenberg
CHEO Consultants:
- Dr. Anton Baksh
- Dr. Hazen Gandy, Medical Director
- Dr. Marijana Jovanovic
- Dr. Marina Moharib
- Dr. Tea Rosic
- Dr. Sinthuja Suntharaligam
Vanier Consultants:
- Dr. Simran Ahluwalia
- Dr. Sarah Armstrong
- Dr. Sohail Makhdoom
- Dr. Rida Mirza
- Dr. Syed Naveed Rizvi, Medical Director
- Dr. Margaret Steele
- Dr, Javeed Sukhera
- Dr. Richard Zayad

Becoming a Safe Provider for All
Created in collaboration with Public Health Agency of Canada, SickKids and the Community. Gender identity development starts in childhood and we all have a responsibility to create safe, inclusive spaces for all children, their families and providers across all sectors. This webinar series was developed with input from Cathy Maser, a nurse practitioner with years of experience working with children and youth and Donna De Filippis, parent of a transgender young women to provide information and support to enable all of us to create gender affirming spaces. The content was created and will be delivered by community members who are educators and providers in Indigenous and 2SLGBTQ+ agencies across the country, with a specific focus on gender diverse children.- Session 1: Becoming a Safe Provider , Becoming a Safe Provider (PDF)
- Session 2: Being Affirming , Being Affirming (PDF)
- Session 3: Barriers to Care, Barriers to Care (PDF)
- Session 4: Moving Forward: Our Stories
Les mots et les actions comptent : Offrir des espaces d’affirmation du genre pour tous
Créé en collaboration avec l’Agence de la santé publique du Canada, SickKids et la collectivité. Le développement de l’identité de genre commence dès l’enfance et nous avons tous la responsabilité de créer des espaces sûrs et inclusifs pour tous les enfants, leurs familles et les fournisseurs de services dans tous les secteurs. Cette série de webinaires a été développée avec la participation de Cathy Maser, infirmière praticienne dotée de plusieurs années d’expérience de travail avec les enfants et les jeunes et Donna De Filippis, mère d’une jeune femme transgenre, pour fournir de l’information et du soutien qui nous permettent à tous de créer des espaces d’affirmation du genre. Le contenu a été créé et sera distribué par des membres de la communauté qui sont des éducateurs et des fournisseurs dans les agences autochtones et 2SLGBTQ+ à travers le pays, avec un accent particulier sur les enfants de diverses identités de genre.
- Séance 1: Devenir un fournisseur de services sûrs, Devenir un fournisseur de services sûrs (PDF)
- Séance 2: Lors de l'enregistrement du webinaire en français, il y a eu quelques problèmes techniques qui ont affecté sa qualité. Malheureusement, le webinaire n'est pas utilisable pour la visualisation et la distribution publique. L'enregistrement de ce webinaire n'est disponible qu'en anglais pour le moment. Être affirmant (PDF)
- Séance 3: Obstacles à l’obtention de soins , Obstacles à l’obtention de soins (PDF)
- Séance 4: Aller de l’avant : Nos histoires
Contact TeleLink
For General Inquiries:
Phone: 1-877-507-7301
Fax: 416-813-2189
telepsychiatry.inquiries@sickkids.ca
For Intake Inquiries:
Phone: 416-813-6503
telepsychiatry@sickkids.ca
Our history
With its origins in the year 2000, TeleLink has evolved from a pioneering videoconference-based program in scope, reach, technological modalities, service offerings, funders, and names.
Originally, TeleLink served only certain children’s mental health agencies designated by the Ministry of Child & Youth Services, for one-time consultations from child psychiatrists and specialist children’s mental health professionals. TeleLink saw its first significant expansion in 2007 with the addition of the Eastern (CHEO) and Western (CPRI) delivery hubs and their surrounding children’s mental health agencies.
In 2011 a further expansion to all children’s mental health providers in non-urban Ontario, followed by an Urban Telemental Health Services pilot to the Greater Toronto Area has positioned TMHS to be a truly pan-provincial program, supporting a variety of primary care providers of child/youth mental health care.

